- Benign Prostatic Hyperplasia (BPH)
- Bladder Cancer
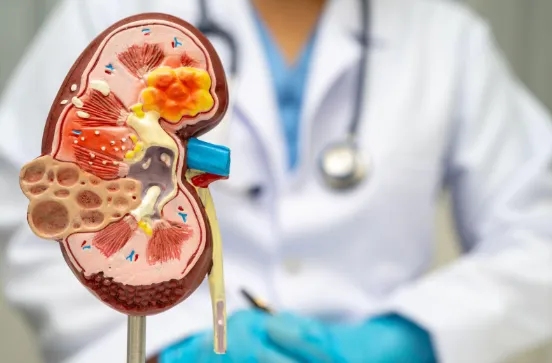
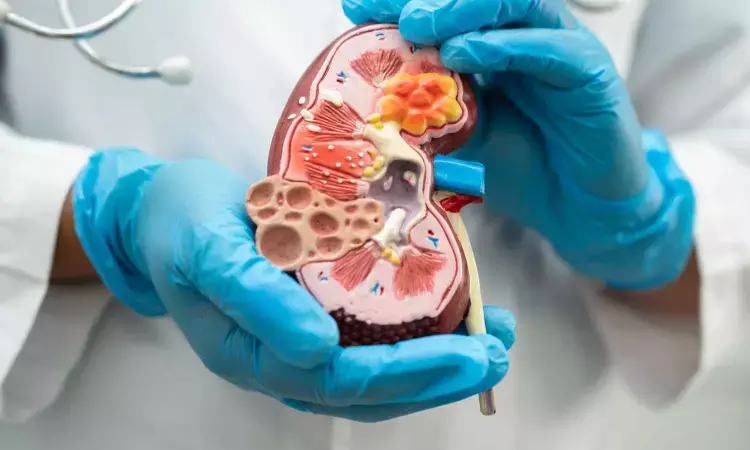
- Kidney Cancer
- Prostate Cancer
- Urolithiasis (Kidney Stones)
- Stress Urinary Incontinence
- Urodynamic Evaluation
- Male Infertility
- Pelvi-Ureteric Junction (PUJ) Obstruction
- Urethral Stricture
- Urinary Fistulas
- Kidney Transplantation
- Urinary Tract Infection
- Erectile Dysfunction
- Overactive Bladder

Benign Prostatic Hyperplasia (BPH)
This is a very common condition affecting males above 50 years of age. Prostate gland is situated around the urethra just below the bladder and in front of the rectum. Enlargement of Prostate manifests as urinary problems like hesitation to start voiding, Poor urinary stream, incomplete sensation of voiding, urgency to pass urine or increased frequency of urination. This can be diagnosed by a digital Rectal Examination. Urinalysis, Ultrasound of kidney Ureter & Bladder (KUB) and estimation of renal function (S.Creatinine & B.Urea) are helpful in evaluation. S.Prostate Specific Antigen (S.PSA) level estimation in blood helps to rule out Prostatic Cancer. Uroflowmetry is essential for the objective evaluation of the urinary stream.
Treatment
Benign Prostatic Hyperplasia (BPH) can be managed by two modalities- Medical or surgical.
-
Medical therapy is with alpha Blockers and 5 alpha reductase inhibitors. These drugs have to be consumed lifelong. Some patients on medical therapy may later have worsening of symptoms or retention of urine. These patients need surgical treatment. Apart from this, patients not relieved by medications and those who don’t want to continue medicines opt for surgical treatment.
-
Transurethral Resection of prostate is the commonly performed procedure. Through an endoscope the enlarged prostate gland is removed in small pieces and washed out. Traditionally it was done using nonphysiological solutions contributing to complications. Now endoscopic resection of prostate can be done with Bipolar TURP using Normal saline which is physiological. This considerably reduces complications and can be safely used for older patients especially those with pacemakers and other co morbidities.
-
This examination is done for examining the prostate gland situated anterior to the rectum. This helps in identifying the diseases in the prostate like Prostatitis, Benign Prostatic Hyperplasia and Carcinoma Prostate.
Patient is positioned in lateral position and a finger is inserted into the rectum to feel the prostate gland. It is not a painful procedure.

Bladder Cancer
Cancer affecting the bladder usually presents with blood in urine (Haematuria). This is why it is very important to consult a Urologist in case of haematuria especially when it occurs without pain. They are often easily detected by an ultrasound scan but smaller tumours may be missed. Patient need a cystoscopy for confirming the diagnosis and biopsy if needed. Contrast enhanced CT scan helps in assessing the extent of the disease.
Treatment
Once diagnosed early bladder tumours can be removed endoscopically (TURBT).
These patients need meticulous follow up for long term after the procedure.
If the tumour is extensive the whole bladder has to be removed (Radical Cystectomy). After that a urine conduit or reservoir is created with patient’s intestine. This can be connected to the urethra or to an opening on the side of abdomen (Urinary Diversion). Depending on the technique of drainage of urine patient may have to use a catheter or a bag. Some patients can be made to void normally through the urethra even after removal of the bladder.
Very rarely only they need chemotherapy or Radiotherapy if diagnosed early.

Kidney Cancer
Kidney cancers are often discovered incidentally during an ultrasound or CT scan done for unrelated reasons. Because of this, many tumors are detected at an early stage. In such cases, it is often possible to remove only the tumor while preserving the rest of the kidney — a procedure called Partial Nephrectomy.
In more complex or advanced cases, however, complete removal of the kidney (Radical Nephrectomy) may be necessary to ensure safe and effective treatment.

Prostate Cancer
Prostate cancer is one of the most common cancers affecting men. The good news is that it can often be detected early with a simple blood test called Serum PSA (Prostate-Specific Antigen), which is widely available.
If the PSA level is elevated, further evaluation is needed. The definitive diagnosis is made through a prostate biopsy, where small tissue samples are examined under a microscope.
Treatment Options
The choice of treatment depends on the type of tumor, its stage, and the patient’s overall health. The main options include:
-
A surgical procedure in which the prostate gland is completely removed. After removal, the bladder is reconnected directly to the urethra to restore urinary continuity.
-
High-energy radiation is used to destroy cancer cells in and around the prostate.
Other options such as active surveillance, hormone therapy, or chemotherapy may also be considered in selected patients, depending on disease stage and aggressiveness.
Urolithiasis
Most urinary stones are formed in the kidney due to crystallization of metabolic products in the body. While some stones remain inside the kidney, others may move down into the ureter (the tube connecting the kidney and bladder).
When stones try to pass through urine, they can cause sudden and severe pain known as Ureteric Colic.
Small stones may pass spontaneously after two or three painful episodes.
Larger or impacted stones often require medical or surgical removal.
If neglected, stones can block urine flow, damage kidney function, and even lead to permanent kidney failure. Hence, regular follow-up and proper management are crucial for patients with urinary stones.
Treatment Options
The choice of treatment depends on the stone’s size, type, and location. Common procedures include:
-
A small endoscope is passed through the urethra into the ureter to directly visualize and fragment stones.
-
A minimally invasive procedure where stones inside the kidney are removed through a small incision at the back.
-
Uses a flexible endoscope passed through the urinary tract to reach the kidney and remove stones.
-
Non-invasive technique where shock waves are applied from outside the body to break stones into smaller fragments that pass naturally in urine.

Stress Urinary Incontinence (SUI)
Stress Urinary Incontinence is the leakage of urine during activities that increase pressure inside the abdomen, such as coughing, sneezing, laughing, exercising, or lifting heavy weights.
It is more common in women, especially after pregnancy and childbirth, which can weaken the muscles and support structures of the bladder and urethra.
Diagnosis & Evaluation
A proper evaluation by a urologist is essential to confirm the type of incontinence and rule out other causes. This usually includes:
- Detailed medical history
- Physical examination
- Simple urine tests
- Specialized studies if required (urodynamics)
Treatment Options
-
Pelvic floor exercises (Kegel’s), weight reduction, and bladder training.
-
May help in selected patients.
-
The most effective and widely performed treatment is Vaginal Tape Surgery (e.g., TVT/TOT), where a supportive sling is placed under the urethra to prevent leakage. With modern techniques, surgery is minimally invasive, safe, and offers excellent long-term results.

Urodynamic Evaluation
Urodynamic Evaluation is a diagnostic test that measures how well the bladder and urethra store and release urine.
It records the pressure changes inside the bladder during both the storage phase (when the bladder is filling) and the emptying phase (when urine is passed).
The procedure is done using a special catheter connected to sensitive pressure sensors and computer software, which analyzes and interprets the results.
Why is it done?
Urodynamic studies help in the diagnosis and management of conditions such as:
- Urinary incontinence (leakage of urine)
- Difficulty in passing urine
- Overactive bladder
- Neurological bladder disorders
This evaluation allows your urologist to choose the most appropriate treatment tailored to your condition.

Male Infertility
Male factors contribute to nearly half of all cases of infertility in couples, yet they are often overlooked. A detailed evaluation by a urologist can help identify the underlying causes and significantly improve the chances of conception.
Common Causes
- Hormonal imbalances
- Sperm production or transport problems
- Varicocele (dilated veins around the testis)
- Genetic or structural conditions
Treatment Options
-
Varicoceles are a common and correctable cause of male subfertility. The preferred method is Subinguinal Varicocelectomy under magnification, which allows preservation of the testicular artery, ligation of abnormal veins, and protection of lymphatic channels.
-
In cases of very low or absent sperm counts, modern sperm retrieval methods can be performed. These help in successful use of Assisted Reproductive Techniques (ART) such as ICSI (Intracytoplasmic Sperm Injection).
Why Evaluation Matters
With timely evaluation and appropriate treatment, male infertility can often be effectively managed, improving the overall success rates of natural conception or assisted methods.

Pelvi-Ureteric Junction (PUJ) Obstruction
PUJ Obstruction is a condition where the normal flow of urine is blocked at the junction between the renal pelvis (part of the kidney that collects urine) and the ureter (tube carrying urine to the bladder).
Key Facts
- It is usually a congenital problem (present from birth).
- The blockage prevents proper drainage of urine from the kidney.
- If left untreated, it can lead to progressive kidney damage and loss of function.
Symptoms
- Recurrent abdominal or flank pain
- Urinary infections
- Swelling of the kidney (hydronephrosis) detected on ultrasound
- Sometimes diagnosed during pregnancy scans or childhood check-ups
Treatment
The standard treatment is surgical repair (Pyeloplasty), which removes the obstruction and restores smooth urine flow. This procedure has very high success rates. In many cases, renal function can be preserved or regained after timely intervention.

Urethral Stricture
A urethral stricture is a narrowing of the urethra (the tube that carries urine from the bladder to the outside). This narrowing blocks the normal flow of urine.
Causes
- Most commonly occurs after injury or trauma to the urethra
- Can also result from previous surgeries, infections, or instrumentation
Symptoms
- Weak or thin urine stream
- Difficulty in passing urine
- Frequent urinary infections
- Incomplete emptying of the bladder
Treatment
-
The commonest method, where the stricture is incised using an endoscope.
-
Instillation of cultured buccal mucosal epithelial cells over the incision site, which may improve healing and reduce recurrence.
-
The standard and most effective treatment, where the narrowed segment is either removed and rejoined, or widened using grafts.
With modern surgical techniques, excellent long-term results can be achieved, restoring normal urinary flow and quality of life.

Urinary Fistulas
A urinary fistula is an abnormal connection between the urinary system (bladder or ureter) and the vagina. This leads to continuous leakage of urine through the vagina, which can be distressing and socially disabling.
Causes
- Most commonly occurs after difficult gynecological surgeries (such as hysterectomy), especially when the uterus or adnexal structures are densely adherent to the bladder or ureter.
- Can also result from obstructed or complicated labor, pelvic infections, or radiation therapy.
Symptoms
- Persistent leakage of urine through the vagina
- Wetness and discomfort
- Secondary infections and skin irritation
Treatment
The definitive management is surgical repair of the fistula. Surgery can be technically challenging due to scarring, adhesions, and other associated pathologies. With modern surgical techniques and careful planning, successful closure and restoration of continence are achievable in the majority of patients.
Kidney Transplantation
Kidney transplantation is the best treatment for patients with end-stage renal failure, where the kidneys can no longer function adequately.
What is done?
A healthy kidney from a donor is surgically placed in the lower part of the abdomen, where it is connected to the recipient’s blood vessels and urinary bladder. The new kidney starts working soon after surgery, producing urine and restoring normal body functions.
Types of Donation
- Living Donor Transplant: A healthy relative donates one of their kidneys voluntarily.
- Deceased Donor Transplant: A kidney is donated by a person after death (with prior consent or family approval).
After Transplant
Patients usually experience a dramatic improvement in quality of life compared to dialysis. Long-term use of immunosuppressive medicines is essential to prevent rejection of the new kidney. With proper follow-up and medication, many patients enjoy normal, productive lives for decades after a transplant.

Urinary Tract Infection (UTI)
UTI is one of the commonest urinary problems, affecting both men and women. It usually presents with burning sensation while passing urine, increased frequency, urgency, lower abdominal discomfort, or sometimes fever with chills.
Diagnosis
Diagnosis is made through urine analysis and urine culture, which helps in identifying the causative organism and selecting the right antibiotic.
Treatment
Most cases respond well to antibiotics when taken for an adequate duration as advised by a urologist. Recurrent infections, especially in women, require further evaluation to identify underlying causes such as stones, obstruction, or diabetes.
Proper hydration and maintaining good personal hygiene are important preventive measures.

Erectile Dysfunction (ED)
Erectile Dysfunction is the persistent inability to achieve or maintain an erection sufficient for satisfactory sexual activity. It is a common problem affecting men of all ages, though incidence increases with age.
Causes
- Vascular problems (reduced blood flow to the penis)
- Diabetes and hypertension
- Neurological causes
- Psychological issues (stress, anxiety, depression)
- Hormonal imbalance
- Side effects of medications
Treatment
- Lifestyle changes and counseling
- Oral medications (PDE-5 inhibitors)
- Hormonal treatment if deficient
- Vacuum erection devices
- Penile injections or intraurethral therapy
- Penile implant surgery in refractory cases
With modern treatments, the majority of men can regain satisfactory sexual function.

Overactive Bladder (OAB)
Overactive Bladder is characterized by frequent and urgent need to pass urine, with or without urge incontinence (leakage of urine before reaching the toilet). It can significantly affect quality of life.
Causes
- Idiopathic (no identifiable cause)
- Neurological disorders (e.g., stroke, spinal cord disease)
- Bladder outlet obstruction (such as prostate enlargement)
Diagnosis
Diagnosis is made based on clinical history, urine analysis, ultrasound, and urodynamic studies if required.
Treatment
- Behavioral therapy — bladder training, timed voiding, fluid management
- Medications — anticholinergics and beta-3 agonists
- Botulinum toxin injections into the bladder wall for refractory cases
- Neuromodulation techniques in selected patients
